# The Autoimmune-Nutrition Connection: A Comprehensive Guide to Dietary Strategies for Managing Autoimmune Diseases
Autoimmune diseases, a diverse group of chronic conditions affecting millions worldwide, arise when the body’s immune system mistakenly attacks its own healthy tissues. From rheumatoid arthritis and lupus to multiple sclerosis and inflammatory bowel disease, the symptoms and affected systems vary widely, yet a common thread increasingly recognized by researchers and clinicians alike is the profound impact of nutrition on disease progression and management. While medication plays a crucial role, dietary interventions offer a powerful, complementary avenue for reducing inflammation, modulating immune responses, restoring gut health, and improving overall well-being. This extensive guide delves into the intricate relationship between nutrition and autoimmune diseases, offering evidence-based strategies and practical advice for navigating this complex landscape.
Understanding Autoimmunity and the Role of Diet
At its core, autoimmunity is a breakdown of immune tolerance. Genetic predispositions, environmental triggers, and lifestyle factors all contribute to this aberrant immune response. While the exact mechanisms are still being unravelled, accumulating evidence points to the gut as a central player. The gut microbiome – the trillions of microorganisms residing in our intestines – significantly influences immune development and function. Dysbiosis, an imbalance in the gut microbiota, can compromise the integrity of the gut lining (often referred to as “leaky gut” or increased intestinal permeability), allowing undigested food particles, toxins, and microbes to enter the bloodstream and trigger systemic inflammation and immune reactions.
Diet, being the primary modulator of the gut microbiome, therefore holds immense power in either exacerbating or ameliorating autoimmune conditions. Certain foods can be pro-inflammatory, contribute to gut dysbiosis, and perpetuate immune overactivity, while others possess anti-inflammatory properties, support gut health, and help restore immune balance.
Foundational Principles: Core Dietary Strategies
While specific dietary approaches may vary depending on the autoimmune condition and individual sensitivities, several foundational principles underpin effective nutritional interventions for autoimmune diseases.
1. Eliminating Inflammatory Foods

The cornerstone of an autoimmune-friendly diet often begins with the rigorous removal of foods known to promote inflammation and gut dysbiosis.
Gluten
For many individuals with autoimmune conditions, gluten, a protein found in wheat, barley, and rye, can be a significant trigger. Beyond celiac disease, a well-established autoimmune condition triggered by gluten, growing research suggests a link between non-celiac gluten sensitivity and various autoimmune manifestations. Gluten can increase intestinal permeability and activate immune responses in susceptible individuals. A trial elimination of gluten for a period of 4-8 weeks, followed by careful reintroduction, can help identify its role in an individual’s symptoms.
Dairy
:max_bytes(150000):strip_icc()/what-is-the-autoimmune-protocol-diet-heres-what-a-dietitian-has-to-say-757eed4806194e9f88f1fc288d4b5b5a.jpg)
Dairy products, particularly those from cow’s milk, contain proteins like casein and whey that can be allergenic and inflammatory for some people. Lactose intolerance is also common, leading to digestive distress. Similar to gluten, a dairy-free trial can be beneficial to assess individual sensitivity.
Processed Foods, Refined Sugars, and Artificial Ingredients
These ubiquitous components of the modern Western diet are highly pro-inflammatory. Refined sugars fuel pathogenic bacteria in the gut, contributing to dysbiosis, while processed foods are often laden with unhealthy fats, artificial additives, and low nutritional value, all of which can exacerbate inflammation and compromise immune function. Prioritizing whole, unprocessed foods is paramount.
Inflammatory Oils (High Omega-6)
Many processed foods and restaurant meals contain excessive amounts of omega-6 fatty acids from vegetable oils like corn, soy, sunflower, and safflower oil. While omega-6s are essential, an imbalance with omega-3 fatty acids (found in fatty fish, flaxseeds) promotes inflammation. Shifting the dietary fat profile towards healthier, anti-inflammatory sources is crucial.
2. Emphasizing Anti-Inflammatory and Nutrient-Dense Foods
Once inflammatory triggers are removed, the focus shifts to nourishing the body with foods that actively reduce inflammation, support immune regulation, and provide essential nutrients for healing.
Abundant Fruits and Vegetables
These vibrant foods are packed with antioxidants, vitamins, minerals, and phytochemicals that combat oxidative stress and inflammation. Aim for a wide variety of colors to ensure a broad spectrum of nutrients. Organic produce is preferred to minimize exposure to pesticides.
Omega-3 Fatty Acids
Omega-3s, particularly EPA and DHA found in fatty fish like salmon, mackerel, and sardines, are potent anti-inflammatory agents. They help modulate immune responses and reduce the production of inflammatory mediators. Plant-based sources like flaxseeds, chia seeds, and walnuts provide ALA, which the body can convert to EPA and DHA, albeit less efficiently.
Lean Protein Sources
Adequate protein is essential for tissue repair, enzyme production, and immune cell function. Opt for lean, high-quality protein sources such as pasture-raised poultry, grass-fed meats (in moderation), wild-caught fish, and legumes (if tolerated).
Healthy Fats
Include monounsaturated fats from avocados and olive oil, and saturated fats from coconut oil (in moderation), which can be beneficial for cellular health and satiety.
3. Supporting Gut Health: The Gut-Autoimmune Axis
Given the central role of the gut in autoimmunity, strategies specifically aimed at restoring gut integrity and balance are critical.
Probiotic-Rich Fermented Foods
Fermented foods like sauerkraut, kimchi, kefir (dairy or non-dairy), and kombucha introduce beneficial bacteria to the gut, helping to rebalance the microbiome and enhance digestive health. Start with small amounts and gradually increase as tolerated.
Prebiotic Fibers
Prebiotics are non-digestible fibers that feed beneficial gut bacteria. Sources include garlic, onions, leeks, asparagus, bananas (green), and jicama. Incorporating these foods supports the growth of a healthy gut microbiome.
Bone Broth
Rich in collagen, gelatin, and amino acids like glutamine, bone broth is renowned for its gut-healing properties. It can help soothe the intestinal lining, reduce inflammation, and support tissue repair.
Soluble and Insoluble Fiber
A diverse intake of fiber from fruits, vegetables, legumes, and whole grains (if tolerated) is vital for promoting regular bowel movements and nourishing the gut microbiome.
Specialized Dietary Approaches for Autoimmune Disease
Beyond the foundational principles, several structured dietary approaches have gained traction in the management of autoimmune diseases.
1. The Autoimmune Protocol (AIP) Diet
The AIP diet is an elimination and reintroduction diet specifically designed to reduce inflammation, heal the gut, and identify individual food triggers in autoimmune conditions. It is more restrictive than a general anti-inflammatory diet and typically involves:
Elimination Phase
Strict removal of grains (including gluten and non-gluten grains), legumes, dairy, eggs, nuts, seeds (including coffee and spices derived from seeds), nightshade vegetables (tomatoes, potatoes, peppers, eggplant), refined sugars, processed foods, alcohol, and NSAIDs. This phase is typically followed for 30-90 days or until significant symptom improvement is observed.
Reintroduction Phase
Foods are systematically reintroduced one at a time, with careful monitoring of symptoms. This meticulous process helps individuals identify their specific trigger foods. The AIP diet is not intended as a long-term restrictive diet, but rather a tool to gain valuable insights into individual food sensitivities.
2. Paleo Diet (Modified)
The Paleo diet emphasizes whole, unprocessed foods that were presumably available to our Stone Age ancestors. It typically excludes grains, legumes, dairy, refined sugars, and processed foods. For autoimmune conditions, a modified Paleo approach often incorporates elements of the AIP, particularly the avoidance of nightshades, eggs, and nuts, until individual tolerance is established.
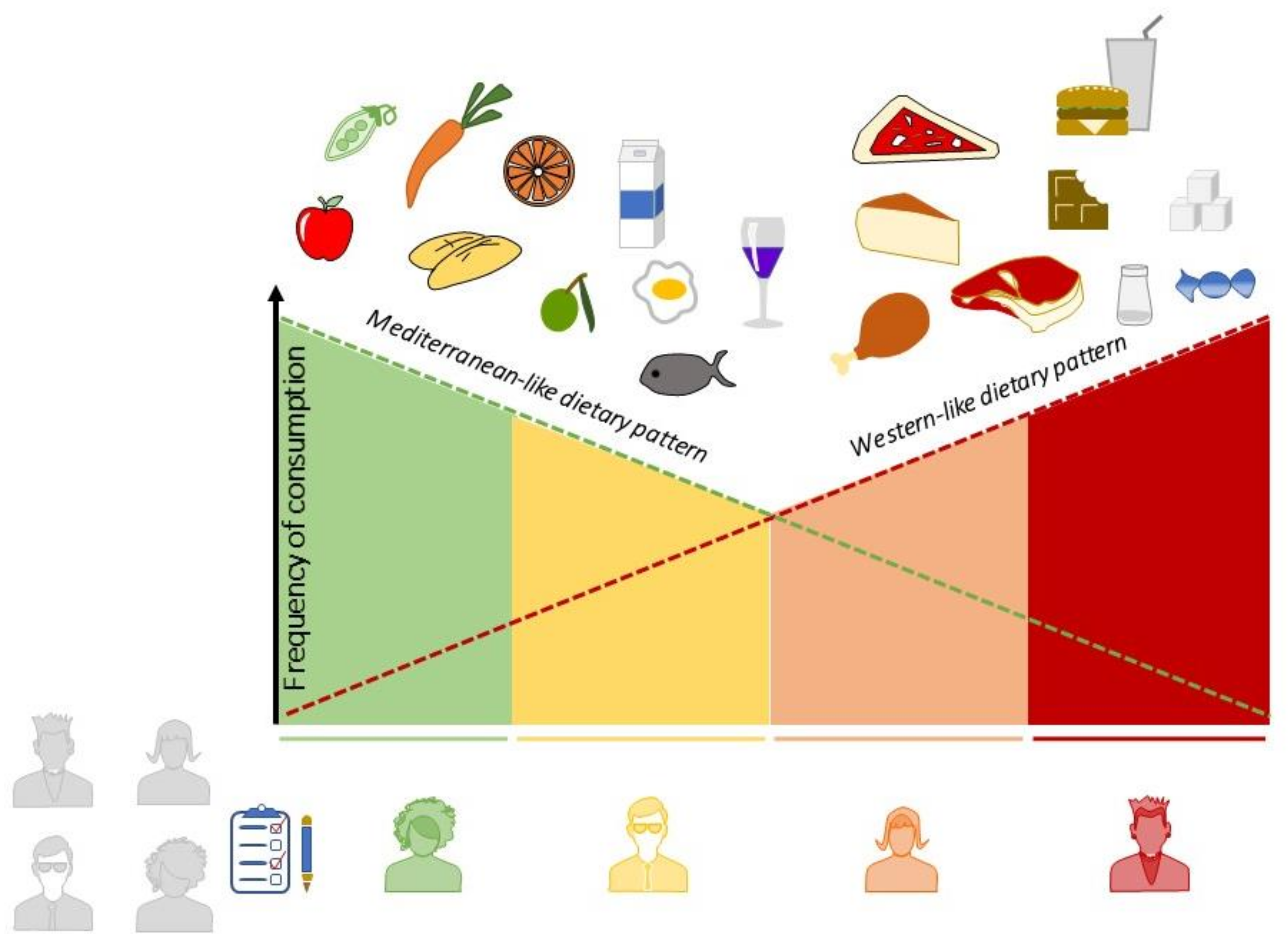
3. Mediterranean Diet (Anti-inflammatory Focus)
While not specifically designed for autoimmunity, the Mediterranean diet aligns well with anti-inflammatory principles. It emphasizes whole grains (often tolerated by some, but can be modified to be grain-free), abundant fruits and vegetables, legumes, nuts, seeds, olive oil as the primary fat source, and moderate amounts of fish, poultry, and dairy. Red meat is consumed sparingly. Its emphasis on plant-based foods, healthy fats, and lean protein makes it a sustainable and beneficial approach for many.
4. Specific Carbohydrate Diet (SCD)
The SCD is a grain-free, lactose-free, and sucrose-free diet that aims to reduce inflammation and promote gut healing in individuals with inflammatory bowel disease (IBD) and other digestive disorders. It focuses on easily digestible carbohydrates and excludes complex carbohydrates that can feed pathogenic bacteria. While originally for IBD, some individuals with other autoimmune conditions find benefit from its principles.
Important Considerations and Practical Advice
Implementing significant dietary changes for autoimmune diseases requires commitment, patience, and often, professional guidance.
Work with a Qualified Healthcare Professional
Given the complexity of autoimmune diseases and individual variations, it is highly recommended to work with a healthcare professional experienced in functional medicine or a registered dietitian nutritionist specializing in autoimmune conditions. They can help tailor a diet plan, monitor progress, address nutrient deficiencies, and ensure nutritional adequacy.
Patience and Consistency
Dietary changes do not typically yield immediate results. It can take weeks or even months to observe significant improvements. Consistency is key, and setbacks are normal. Focus on long-term sustainable changes rather than quick fixes.
Addressing Nutrient Deficiencies
Individuals with autoimmune diseases are often prone to nutrient deficiencies due to malabsorption, increased nutrient demands, or dietary restrictions. Common deficiencies include Vitamin D, B12, magnesium, zinc, and omega-3 fatty acids. Targeted supplementation, guided by laboratory testing and professional advice, may be necessary.
Stress Management
Stress profoundly impacts the immune system and gut health. Chronic stress can exacerbate inflammation and worsen autoimmune symptoms. Incorporating stress-reducing practices like mindfulness, meditation, yoga, or spending time in nature is an integral part of a holistic approach to managing autoimmune disease.
Adequate Sleep
Sleep is crucial for immune regulation and overall healing. Aim for 7-9 hours of quality sleep per night. Poor sleep can increase inflammation and impair immune function.
Hydration
Staying well-hydrated is essential for all bodily functions, including detoxification and nutrient transport. Drink plenty of filtered water throughout the day.
Food Quality Matters
Whenever possible, choose organic, pasture-raised, grass-fed, and wild-caught options to minimize exposure to hormones, antibiotics, pesticides, and other toxins that can contribute to inflammation.
Listen to Your Body
Every individual is unique, and what works for one person may not work for another. Pay close attention to how your body responds to different foods and adjust your diet accordingly. Keeping a food and symptom journal can be incredibly helpful in identifying patterns.
The Future of Autoimmune Nutrition
Research into the interplay between diet, the microbiome, and autoimmunity is rapidly evolving. Emerging areas of interest include:
Personalized Nutrition
With advancements in genomics and microbiome analysis, the future of autoimmune nutrition is likely to involve highly personalized dietary recommendations based on an individual’s unique genetic makeup and gut microbiome profile.
Specific Micronutrients and Bioactives
Further research is exploring the precise roles of specific vitamins, minerals, and bioactive compounds in modulating immune responses and reducing inflammation in autoimmune conditions.
Therapeutic Fasting
While still an area of active research, intermittent fasting and longer therapeutic fasts are being investigated for their potential to induce autophagy (cellular clean-up), reduce inflammation, and promote gut healing.
Conclusion
The connection between nutrition and autoimmune diseases is undeniable and increasingly recognized as a cornerstone of comprehensive management. By strategically eliminating inflammatory triggers, embracing nutrient-dense and anti-inflammatory foods, and actively supporting gut health, individuals with autoimmune conditions can significantly impact their symptoms, improve their quality of life, and potentially slow disease progression. While dietary changes require dedication and often professional guidance, the profound benefits of taking an active role in one’s health through nutrition offer immense hope and empowerment in navigating the challenges of autoimmune disease. As research continues to unfold, the power of food as medicine will undoubtedly play an even greater role in shaping the future of autoimmune care.

:max_bytes(150000):strip_icc()/EW-Meal-Plans-Healthy-Weight-Gain-Day-4-1x1-alt-81577102cff74485ac146541976d8b22.jpg?resize=200,135&ssl=1)

